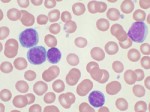
Considering Evidence for a New Drug for Immune Thrombocytopenia Purpura
I’ve been wondering, lately, why so many of the medical blogs cover the same topics, like last week’s lung cancer detection trial, which are often the exact same studies as are reported by conventional news outlets. I’ve been trying, here, to sometimes consider new published articles that seem important to me but, for whatever reasons, don’t get so much attention.
Here’s one:
Yesterday’s NEJM includes an article Romiplostim or Standard of Care in Patients with Immune Thrombocytopenia.* It’s about a drug, manufactured and sold by Amgen as NPlate, that received FDA approval for treatment of chronic immune thrombocytopenia purpura (ITP) in August, 2008. Some consider ITP a rare disease, and