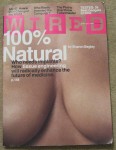
After Breast Cancer, Get a Gym Membership!
The findings show that it’s safe for women who’ve had breast cancer surgery to work out in a way that includes a careful, progressive upper body strengthening. Weight lifting is not only safe; it can reduce lymphedema in women at risk. But “old wives’ tales” still persist in some doctors’ minds and established medical resources. These need be dispelled.