Harlem Hospital Center stands just three miles or so north of my home. I know the place from the outside glancing in, as you might upon exiting from the subway station just paces from its open doors. The structure seems like one chamber of its neighborhood’s heart; within a few long blocks’ radii you’ll find rhythms generated in the Abyssinian Baptist Church; readings at the Schomburg Center and artery-clogging cuisine at the West 135th Street IHOP.
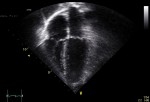
So I was saddened to hear about the missed heart studies. Or should I say unmissed? No one noticed when nearly 4,000 cardiac tests went unchecked at the Harlem center,
Posted in Cardiology, Communication, health care costs, health care delivery, Ideas, Life in NYC, Medical News, Patient Autonomy, Under the RadarTagged communicating in medicine, echocardiograms, Harlem Hospital, health, health care costs, hospital administration, medical tests, test reports