Eight Years
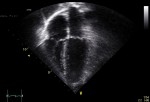
Today marks exactly eight years since Dr. L., the fine radiologist who may have saved my life, called to let me know about my breast cancer diagnosis. With deep-felt thanks to my doctors, my friends, my family, ES Related Posts:Breakfast Will Never Be the Same AgainLiving Like It’s Shark Week, Take 3The Iron Lady, a […]