Reducing Cancer Care Costs: Why Not Offer Neulasta in Smaller Vials?
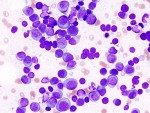
This is the fifth in a series of posts on how we might reduce the costs of cancer care, based on 10 suggestions offered in a May, 2011 NEJM sounding board. We’re up to point 4: oncologists should replace the routine use of white-cell-stimulating factors with a reduction in the chemotherapy dose in metastatic solid cancers. In […]