I first heard about STI-571 (Gleevec, a targeted cancer therapy) from a cab driver in New Orleans in 1999. “Some of the doctors told me there’s a new cure for leukemia,” he mentioned.
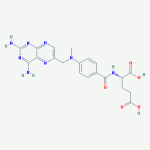
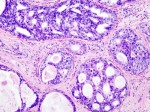
We were stuck in traffic somewhere between the airport and the now-unforgettable convention center. His prior fare, a group of physicians in town for the American Society of Hematology’s annual meeting, spoke highly of a promising new treatment. It seemed as if he wanted my opinion, to know if it were true. Indeed, Dr. Brian Druker gave a landmark plenary presentation on the effectiveness of STI-571 in patients with chronic myelogenous leukemia (CML) at the conference. I was aware of the study findings.
“Yes,” I said. “There is a new drug for leukemia.”
Since then, oncologists’ enthusiasm for targeted therapies – medications designed to fight cancer directly and specifically – has largely held. But the public’s enthusiasm is less apparent. Perhaps that’s because many people are unaware of these new drugs’ potential, or they’re put off by their hefty price tags.
Posted in cancer treatment, Oncology (cancer), Selected TopicsTagged cancer medicine, cancer treatment, Gleevec, health, health care costs, monoclonal antibodies, Oncology (cancer), Sutent, targeted therapy