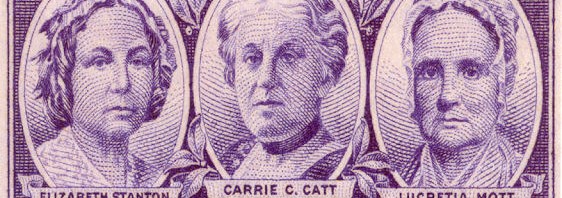
A Visit to Suffragette City
For two days I’ve been traveling on a short road-trip with my family in Upstate New York. As far as this turning to a medical lesson, all I can say is that for the first time in my life I witnessed, first-hand, the vaguely digital, elongate and eponymous geography of the fine Finger Lakes…